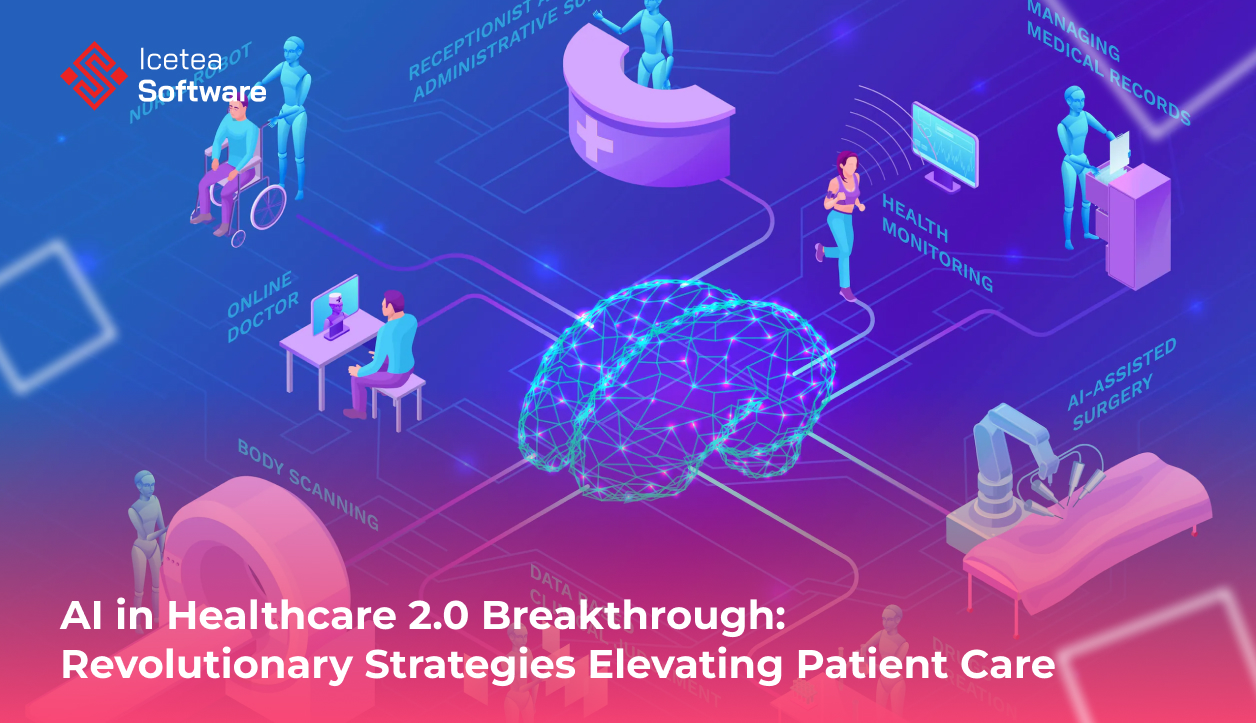
AI in Healthcare 2.0 Breakthrough: Revolutionary Strategies Elevating Patient Care
Artificial Intelligence (AI) is no longer a futuristic buzzword confined to science fiction—it has become an indispensable tool in modern medicine, quietly transforming every facet of healthcare delivery. From the earliest forays into expert systems in the 1980s to today’s deep‑learning algorithms that rival human specialists, AI’s evolution mirrors the healthcare industry’s own progression toward data‑driven, patient‑centered care. Yet despite its promise, healthcare lags behind other sectors in AI adoption, hindered by regulatory complexities, integration challenges, and concerns over data privacy and bias. With an estimated 4.5 billion people worldwide still lacking access to essential health services and a projected shortage of 11 million health workers by 2030, the imperative to harness AI’s potential has never been greater.
This article explores six of the most impactful ways AI is reshaping healthcare today—drawing on real‑world examples, key milestones, and the critical hurdles that must be overcome to ensure these technologies benefit patients equitably.
1. From Rule‑Based Expert Systems to Deep Learning: The Evolution of Diagnostic AI
The journey of AI in healthcare began with rule‑based expert systems in the 1970s and 1980s. These “if‑then” engines encoded domain knowledge—laboriously crafted by human experts—into a network of logical rules. Early systems like MYCIN demonstrated that computers could rival physicians in specific diagnostic tasks (e.g., identifying bacterial infections), but they faltered when medical knowledge changed or grew too complex. Updating hundreds or thousands of interlocking rules proved unwieldy.
The true leap forward came with machine learning (ML) and, more recently, deep learning (DL). Instead of hand‑crafted rules, ML systems learn patterns directly from data—patient records, radiology images, genomic sequences. Deep neural networks, inspired by the human brain, excel at recognizing intricate visual patterns and complex relationships in large datasets.
- Stroke detection: In landmark trials, a deep‑learning model trained on thousands of head CT scans has achieved nearly double the accuracy of expert radiologists in identifying acute stroke lesions and estimating the time of onset—vital information for determining eligibility for clot‑busting treatments within narrow therapeutic windows.
- Cancer screening: Google’s DeepMind and other research teams have developed DL algorithms that outperform human readers in breast and lung cancer screening, reducing both false positives and false negatives. In some studies, AI systems detected cancers up to six months earlier than conventional radiology reads.
- Ophthalmology and pathology: AI‑powered retinal image analysis can now flag early signs of diabetic retinopathy, glaucoma, and age‑related macular degeneration. Digital pathology platforms use convolutional neural networks to classify tumor subtypes and grade disease severity with consistency that rivals or surpasses experienced pathologists.
This evolution from brittle rule‑based engines to adaptive, data‑driven algorithms has ushered in a new era of diagnostic precision—one in which AI serves as a tireless “second reader,” reducing diagnostic errors, speeding up workflows, and ultimately saving lives.
2. Accelerating Emergency Response and Triage
When minutes count, AI can be the difference between life and death. Emergency medical services (EMS) and hospital emergency departments are under relentless pressure—overcrowding, staffing shortages, and uneven resource distribution all compromise patient outcomes. AI‑powered solutions are beginning to streamline these high‑stakes environments:
- Ambulance triage: In the UK’s Yorkshire region, an AI model trained on paramedic records and vital sign data (heart rate, mobility, oxygen saturation, chest pain) accurately predicted the need for hospital admission in 80 percent of cases. By distinguishing high‑risk patients from those safe to manage at home, AI helps prioritize ambulance dispatch, reduce unnecessary transports, and free up critical resources for life‑threatening emergencies.
- Pre‑hospital stroke alerts: Mobile stroke units equipped with AI‑enhanced CT scanners can analyze brain images on the spot, relaying results to neurologists en route. This capability cuts door‑to‑needle times by up to 30 percent, ensuring faster delivery of thrombolytic therapies and improving functional outcomes.
- Emergency department flow: AI tools ingest real‑time patient data (triage notes, room availability, staffing levels) to forecast surges in patient volume and dynamically allocate beds, staff, and equipment. Hospitals using such predictive analytics report 15–25 percent reductions in wait times and significant improvements in patient satisfaction.
By embedding AI into the earliest moments of care, health systems can orchestrate a more efficient, agile, and equitable emergency response—ultimately reducing morbidity and mortality for patients in critical condition.
3. Foreseeing Illness: Predictive and Preventive Healthcare
Perhaps the most transformative promise of AI lies in its ability to anticipate disease before patients ever show symptoms. Traditional medicine often operates in reactive mode—treating illnesses after they manifest. AI‑driven predictive models, however, shift the paradigm toward proactive prevention:
- Chronic disease risk scoring: Large‑scale studies using health record data from half a million patients in the UK have demonstrated AI’s ability to predict the onset of over 1,000 conditions—including Alzheimer’s disease, chronic obstructive pulmonary disease (COPD), kidney failure, and cardiovascular events—years before clinical presentation.
- Genomic and multi‑omics integration: AI algorithms can parse genomic, proteomic, and metabolomic data to identify molecular signatures that herald disease, enabling personalized screening schedules. For example, in hereditary cancer syndromes, AI‑derived risk models recommend tailored imaging frequency, balancing early detection against radiation exposure.
- Digital biomarkers & wearables: Continuous data streams from wearable devices—heart rate variability, sleep patterns, activity levels—feed AI systems that detect subtle deviations from individual baselines. Early trials show this approach can predict Parkinson’s disease motor fluctuations, detect atrial fibrillation, and even forecast mood relapses in bipolar disorder.
By marrying vast biomedical datasets with advanced analytics, AI is ushering in an era of truly precision prevention—one in which interventions can occur at the very inception of disease, improving outcomes and reducing the long‑term burden on healthcare systems.
4. Enhancing Clinical Decision Support and Workflow Efficiency
Beyond diagnostics and prediction, AI is streamlining everyday clinical operations and decision‑making, helping clinicians manage information overload and focus on patient care:
- Contextual clinical notes: Ambient AI systems like Microsoft’s Dragon Ambient eXperience Copilot passively listen to doctor‑patient interactions and generate structured clinical documentation, reducing note‑taking time by up to 50 percent. This not only mitigates physician burnout but also improves documentation completeness and coding accuracy.
- Evidence‑based treatment recommendations: AI platforms can synthesize the latest clinical guidelines, trial data, and individual patient factors (comorbidities, allergies, prior responses) to propose tailored treatment plans. Early adopters report 20–30 percent faster care planning and increased adherence to best‑practice protocols.
- Automated imaging workflows: In radiology, AI‑driven worklists prioritize critical studies (e.g., suspected intracranial hemorrhages, pulmonary embolisms), ensuring these cases jump to the front of the queue. Studies show this approach reduces turnaround times by 40 percent without compromising report quality.
- Operational analytics: Hospital operations benefit from AI‑powered dashboards that forecast bed occupancy, staffing needs, supply utilization, and potential bottlenecks. Institutions using these tools achieve 10–15 percent improvements in resource utilization and marked reductions in waste.
In an era where clinicians spend more time on screens than at the bedside, AI’s ability to lift mundane cognitive burdens and organize complex information flows is critical to restoring the human heart of medicine.
5. Democratizing Access: Virtual Assistants and Telehealth
A striking paradox of contemporary healthcare is the widening chasm between medical advances and their accessibility. Rural communities, low‑resource settings, and marginalized populations often remain cut off from high‑quality care. AI‑powered digital health platforms are bridging these gaps:
- Conversational agents: Early-generation chatbots struggled with medical nuance, delivering accurate answers only 2–10 percent of the time. Today’s retrieval‑augmented generation (RAG) systems—like ChatRWD—marry large language models with curated medical knowledge bases to achieve around 58 percent accuracy on clinical queries.
- Remote monitoring platforms: Companies like Huma and Biofourmis integrate AI analytics with wearable sensors to monitor heart failure, diabetes, and respiratory illnesses. These platforms have demonstrated 30 percent reductions in hospital readmissions and saved clinicians up to 40 percent of the time spent on data review.
- Tele‑triage and scheduling: AI triage bots can assess symptom severity, recommend next steps (self‑care, primary care, emergency visit), and seamlessly schedule virtual or in‑person appointments—cutting no‑show rates by 15 percent and optimizing provider calendars.
- Language and cultural adaptation: AI translation services and culturally attuned dialogue engines enable real‑time interpretation for non‑English‑speaking patients, improving engagement and adherence in multilingual populations.
By embedding AI into telehealth and digital front doors, health systems can extend the reach of scarce clinical expertise, ensuring that high‑quality guidance and monitoring are not confined to the walls of tertiary centers.
6. Powering Discovery: AI in Research and Drug Development
The drug discovery pipeline has been notoriously slow and expensive—averaging over 10 years and $2 billion to bring a new therapy to market. AI is accelerating this process at every stage:
- Target identification: Deep learning models analyze genomic and proteomic datasets to uncover novel therapeutic targets, particularly in complex diseases like Alzheimer’s and certain cancers.
- Molecular simulation: AI‑based programs such as AlphaFold and RoseTTAFold predict three‑dimensional protein structures with atomic accuracy, resolving challenges that stymied researchers for decades. These insights guide rational drug design and expedite lead optimization.
- Predictive toxicology: AI systems trained on chemical and biological data forecast adverse effects and off‑target interactions, allowing researchers to eliminate problematic compounds early—dramatically reducing late‑stage failures.
- Adaptive clinical trials: AI‑driven trial designs continuously analyze accumulating patient data to refine inclusion criteria, dosages, and endpoints, boosting trial efficiency and increasing the likelihood of success.
Industry projections suggest that by 2025, AI will contribute to 30 percent of new drug discoveries, delivering more personalized and effective therapies to patients faster than ever before.
Navigating Ethical, Regulatory, and Equity Challenges
The exhilarating pace of AI innovation is tempered by equally complex challenges:
- Bias and fairness: AI models trained on historical data risk perpetuating existing disparities—if underserved groups are underrepresented in training datasets, algorithms may underperform for those very populations. Rigorous bias audits and inclusive data collection are non‑negotiable.
- Privacy and security: Patient health information is among the most sensitive data. Ensuring compliance with regulations such as HIPAA, GDPR, and emerging digital health standards requires end‑to‑end encryption, federated learning approaches, and transparent governance.
- Accountability and transparency: When AI systems drive clinical decisions, clear lines of responsibility must be drawn. “Black‑box” models that offer no explainability undermine clinician trust and complicate liability. Explainable AI (XAI) methods are crucial to maintain human oversight and legal clarity.
- Regulatory frameworks: Bodies like the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) are adapting guidance to evaluate AI as a medical device, balancing the need for rigorous validation with a pathway for iterative model improvements.
- Workforce adaptation: Clinicians need education and training in AI literacy—understanding both the capabilities and limitations of these tools—to integrate them responsibly into practice.
Striking the right balance between innovation and safeguards is essential to ensure AI enhances healthcare without exacerbating inequities or compromising safety.
Final Thoughts
Artificial Intelligence stands poised to catalyze one of the most profound transformations in the history of medicine. From the frontlines of emergency response to the depths of genomic research, AI is delivering measurable improvements in diagnostic accuracy, operational efficiency, predictive power, and therapeutic innovation. Yet technology alone will not solve healthcare’s greatest challenges.
The true promise of AI in healthcare lies in collaboration—between data scientists and clinicians, between developers and patients, between regulators and innovators. By embedding ethical principles, rigorous evaluation, and an unwavering focus on equity, we can harness AI’s extraordinary capabilities to build a healthcare ecosystem that is:
- Accessible: Bringing high‑quality care to underserved communities.
- Efficient: Streamlining workflows so clinicians can spend more time with patients.
- Predictive: Detecting disease before it manifests, lowering costs and improving outcomes.
- Personalized: Tailoring prevention and treatment to each individual’s biology and circumstances.
- Transparent: Ensuring AI decisions are explainable, auditable, and accountable.
As we stand at this crossroads, the question is not whether AI will transform healthcare—it already is. The question is how we guide its evolution to amplify human compassion, expertise, and judgment. If we succeed, we will usher in a new golden age of medicine—one in which data‑driven insights and human care converge to deliver better health, well‑being, and dignity for all.
————————————
𝐈𝐜𝐞𝐭𝐞𝐚 𝐒𝐨𝐟𝐭𝐰𝐚𝐫𝐞 – 𝐂𝐮𝐭𝐭𝐢𝐧𝐠 𝐄𝐝𝐠𝐞 𝐓𝐞𝐜𝐡𝐧𝐨𝐥𝐨𝐠𝐢𝐞𝐬
𝐖𝐞𝐛𝐬𝐢𝐭𝐞: iceteasoftware.com
𝐋𝐢𝐧𝐤𝐞𝐝𝐢𝐧: https://www.linkedin.com/company/iceteasoftware/
𝐅𝐚𝐜𝐞𝐛𝐨𝐨𝐤: https://www.facebook.com/IceteaSoftware/
𝐓𝐰𝐢𝐭𝐭𝐞𝐫: https://x.com/Icetea_software